

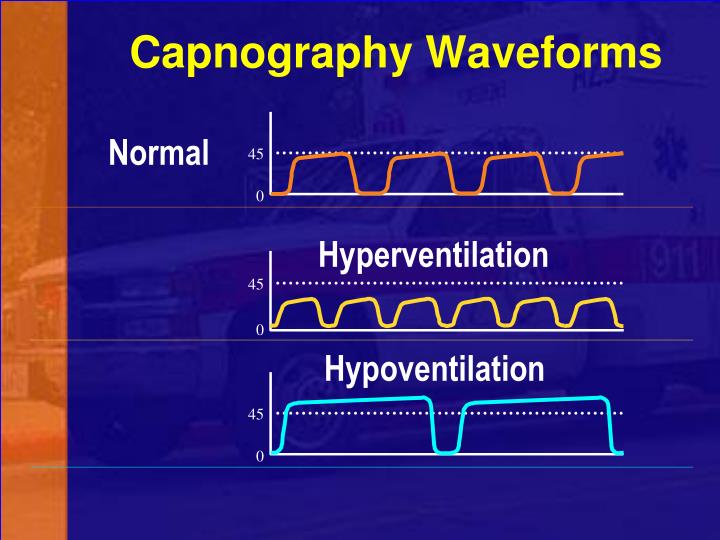
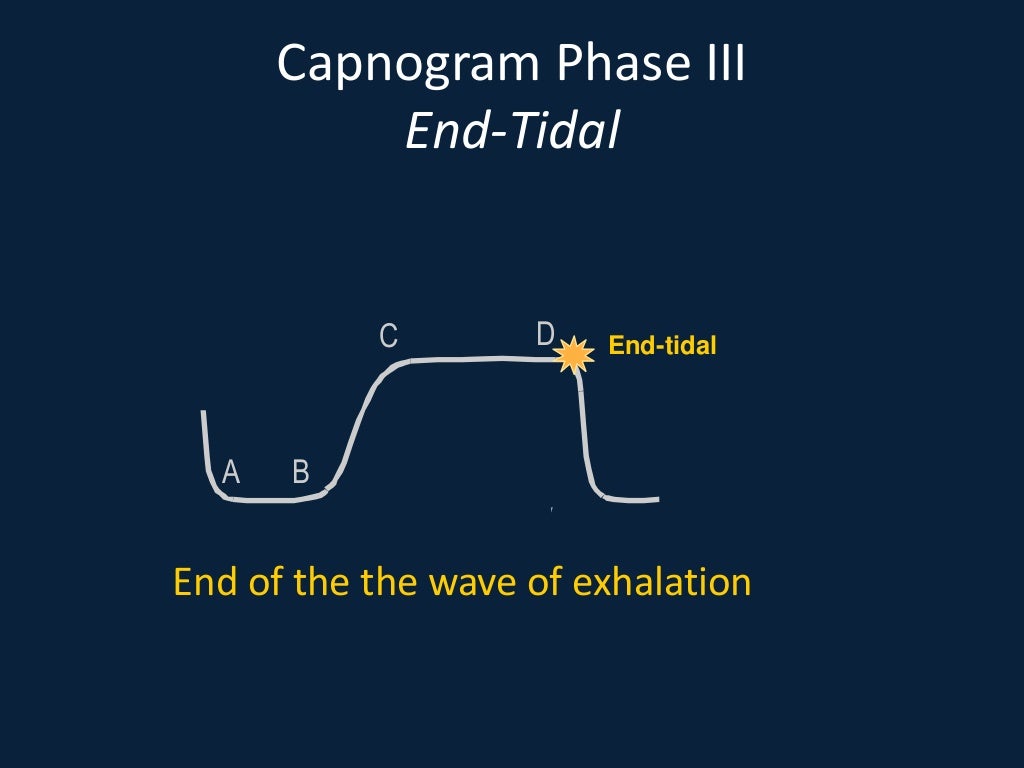
Phase IV (expiratory downstroke) represents the beginning of the next breath, with the CO 2 content returning rapidly to zero. Generally those alveoli with lower / ratios and with longer time constants (containing relatively more CO 2 and emptying relatively slowly) contribute to the later part of phase III, leading to a slight upward slope of the capnography trace. In reality, CO 2 concentrations vary between alveoli as a result of varying ventilation to flow ( /) ratios. Note that if the alveoli all contained exactly the same partial pressure of CO 2, phase III would be completely horizontal. At the end of phase III, the maximal value of CO 2 measured is equivalent to the E′ CO 2. Phase III (alveolar plateau) represents expiration of alveolar gases. Phase II (expiratory upstroke) represents expiration of both dead space gas and alveolar gas from the respiratory bronchioles and alveoli. The end of phase I represents the beginning of expiration, but because the initial gases expired originate from unventilated dead space, the capnography trace remains at zero. Phase I (inspiratory baseline) represents inspiration, and therefore no CO 2 is detected. 1), and is divided into inspiration and expiration: The capnography trace can be described in four stages ( Fig. Reproduced with kind permission from Elsevier (3616430770815).
Physical principles and physiology of capnography In addition, capnography has other uses in ICU relating to airway management and monitoring of respiratory and cardiovascular function. 5 It is well recognized that capnography can be used to detect displaced tracheal tubes and tracheostomy tubes and to diagnose inadvertent oesophageal intubation. Although the use of capnography in ICU has become more widespread since the modification of these guidelines, uptake is still incomplete with only 72% of UK ICUs routinely using capnography. 1 Following the publication of NAP4 in 2011, UK and European guidelines have been modified, 2–4 with the Association of Anesthetists of Great Britain and Ireland (AAGBI) issuing a safety statement in 2011: this stated that continuous capnography should be used in all anaesthetized patients, regardless of the airway device used or the location of the patient, and should be employed in all patients receiving advanced life support.

1 In more than 70% of the deaths in these areas, failure to use capnography in patients dependent on an artificial airway was reported to be a contributory factor. It found that airway complications occurred in the intensive care unit (ICU) and the emergency department (ED) more frequently than in theatres, and that airway events in these areas were much more likely to lead to permanent harm or death. The fourth national audit project (NAP4), a prospective study by the Royal College of Anaesthetists and the Difficult Airway Society, investigated major complications of airway management in the UK. Uses of capnography are wide ranging and not limited to monitoring of the airway
Capnography should be continuously monitored in all patients with an artificial airwayįailure to use capnography in patients dependent on an artificial airway contributed to more than 70% of the ICU-related airway deaths in NAP4Įducation of medical and nursing staff is vital to ensure adequate understanding and appropriate interpretation of the capnography traceĬapnography can be used in both intubated and non-intubated patients


 0 kommentar(er)
0 kommentar(er)
